Watching your loved one go through these changes can be incredibly difficult, especially when you don’t know what lies ahead. In this article, we’ll walk you through the 7 stages of Lewy Body Dementia and help you understand what typically happens in each phase.
What is Lewy Body Dementia?
Lewy Body Dementia is caused by abnormal protein deposits (called Lewy bodies), since the name Lewy body. These deposits interfere with how brain cells communicate, which leads to problems with:
- Attention and Alertness
- Movement and Coordination
- Visual Hallucinations
- Mood, Behaviour, and Sleep
LBD shares some features with both Alzheimer’s and Parkinson’s, but it’s a distinct condition with a unique pattern of symptoms, often starting with fluctuating confusion, movement problems, or hallucinations rather than memory loss.
7 Stages of Lewy Body Dementia:
Lewy Body Dementia (LBD), sometimes called Lewy Body Disease, typically progresses through three broad stages: mild, moderate, and severe.
The journey through LBD is not the same for everyone. Symptoms may appear in different orders or intensities. Since it’s a progressive condition, early diagnosis can really make a difference.
Stage 1: No cognitive decline
Lewy Body Dementia often begins silently. Watch out for signs of anxiety, restlessness. Some people also have trouble falling or staying asleep. There might be occasional forgetfulness or difficulty making decisions.
In terms of movement, slight muscle stiffness or slower walking may show up. You might also notice a light tremor in the hands or fingers, but it’s often subtle.
Stage 2: Mild Cognitive Impairment
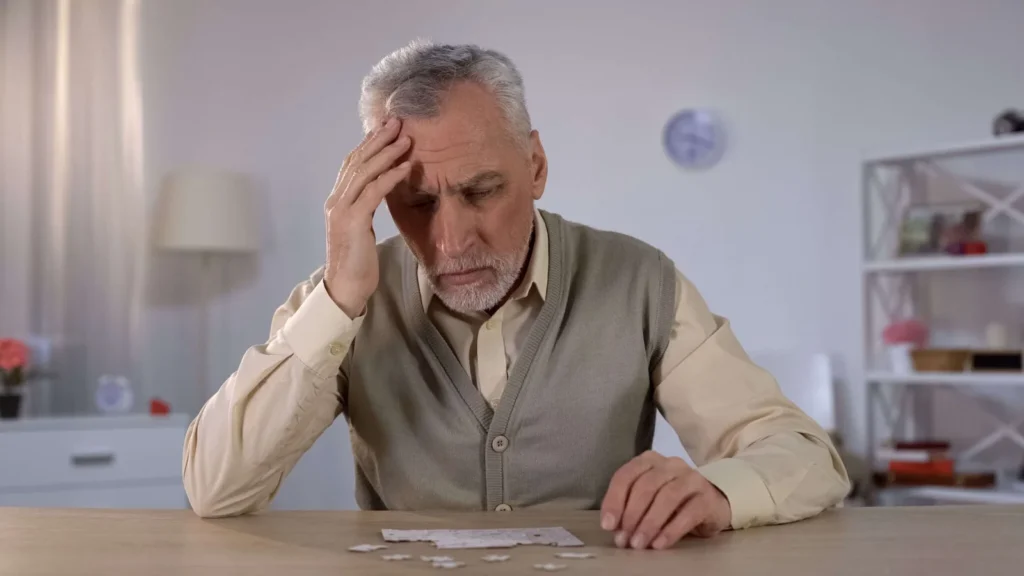
In stage 2 of Lewy Body Dementia, early signs of cognitive decline become more noticeable. This stage is often referred to as mild cognitive impairment (MCI), and the changes may begin to interfere with tasks that require concentration.
A person may have trouble remembering appointments, keeping track of conversations, or solving problems that were once simple. Tasks that require focus — like following a recipe, completing a puzzle, or recalling a list of groceries — may take longer than usual or be forgotten altogether.
Multitasking can also become difficult. The person might get confused when too much is happening at once or become overwhelmed in busy environments. Even though they may still manage on their own at this stage, these difficulties can cause frustration.
Stage 3: Mild Dementia
Stage 3 of Lewy Body Dementia is considered mild dementia. During this stage, the person may begin to show more noticeable changes in thinking and behaviour. They may struggle with memory, decision-making, and using the right words in conversations.
Multitasking becomes harder, and they may feel confused more often, especially in unfamiliar places or situations. Mistakes in judgment, like forgetting to pay bills or missing appointments, may start to happen more regularly.
Changes in mood are also common at this stage. The person may seem more anxious, withdrawn, or disinterested in activities they used to enjoy. They may also show signs of depression or seem emotionally flat.
While many people in this stage can still live on their own, they will need help in managing day-to-day tasks. For example, things like managing money, remembering medications, or organizing their day may require support.
Stage 4: Moderate Dementia
At Stage 4, Lewy Body Dementia progresses into moderate dementia. You may notice the person struggling more with memory, thinking clearly, and using language. Simple daily activities like getting dressed, eating, or bathing can become harder to manage without help.
Changes in mood and behavior also become more common. The person might seem more confused, anxious, or suspicious than before. Despite these challenges, they may still recognize loved ones and hold short conversations.
Read More: How to Encourage Seniors with Dementia to Eat More
Stage 5: Moderately Severe Dementia
In Stage 5, the effects of Lewy Body Dementia become more serious. The person may find it harder to speak clearly, follow conversations, or express their thoughts. Confusion becomes more frequent, and daily tasks like eating, bathing, or dressing often require hands-on help.
They might start having trouble recognizing close family or friends, though they may still respond to familiar voices or routines. Their need for support increases, both physically and emotionally.

Stage 6: Severe Dementia
In Stage 6, Lewy Body Dementia reaches a point where the person becomes almost fully dependent on others. Communication fades, and they may no longer recognize even close family or respond clearly to their surroundings.
Physical decline is also severe — walking, sitting up, or moving without help often becomes impossible. Hallucinations, agitation, and sometimes aggression may appear more frequently, making caregiving more complex and emotionally draining.
Despite these losses, there may be moments of enhanced mental clarity, which is also referred to as mental lucidity. However, this can also signal that the person is in the final stages of the disease.
Read More: Effective Ways to Talk to an Elderly Parent with Dementia
Stage 7: End Stage Dementia
Stage 7 is the final phase of LBD. The person loses most of their memory, language, and physical function. They may no longer speak or move much and are completely dependent on caregivers for daily care, such as feeding, turning, or maintaining hygiene.
This stage is marked by increased confusion, very limited mobility, and near-total loss of independence. It can be emotionally difficult for families, but it’s important to remember that life still holds meaning, even in silence.
People in end-stage dementia may live for many months or years. What matters most during this time is comfort, dignity, and consistent, loving care that brings them peace.
We Help Dementia Patients Maintain Their Quality of Life:
Each type of dementia brings its own challenges for patients and their family members. Managing unique behaviours and communication difficulties—while remaining respectful and supportive—often requires a particular set of skills. At ConsidraCare, we offer in-home care for alzheimers and other types of dementia across the GTA.
We have a dedicated team of nurses and personal support workers who are specially trained in Gentle Persuasive Approaches. This equips them to manage the complications and changes of the disease with dignity and compassion.
Talk to the care advisor today!

Final Thoughts:
Lewy Body Dementia can be overwhelming — not just because of how it affects the person living with it, but also because it’s difficult for families to watch their loved one change.
One of the best things you can do to help a loved one with dementia is to educate yourself about the complexities of the condition. Make use of trusted online resources so you have a clear idea of what to expect. Having that knowledge will also help you plan better care and ensure your loved one gets the support they need.
FAQ’s
1. How long does each stage of Lewy Body Dementia last?
Each stage can vary. Some may last months, others for years. On average, LBD progresses over 5 to 8 years after diagnosis.
2. Are hallucinations always present in LBD?
Visual hallucinations are very common in LBD and often appear early in the disease. They are usually vivid and detailed, like seeing animals or people who aren’t there. Not everyone experiences them, but most do. Hallucinations involving sound or touch can happen, too, but they’re less frequent.
3. What’s the difference between LBD and Alzheimer’s disease?
LBD and Alzheimer’s are both forms of dementia, but they show up differently. Alzheimer’s mainly affects memory early on. LBD tends to impact attention, movement, and alertness first. People with LBD often have hallucinations and Parkinson’s-like symptoms, which are rare in early Alzheimer’s.
4. Is Lewy Body Dementia hereditary?
Lewy Body Dementia isn’t usually inherited. Most cases happen without a clear genetic cause. That said, having a family history of LBD or Parkinson’s might slightly raise the risk. Rare genetic mutations, like those in the SNCA or APOE genes, have been linked to LBD, but these are uncommon.
5. What is the 3-minute test for Lewy Body Dementia?
The 3-minute test is a quick screening tool made up of 10 yes-or-no questions. Six questions focus on non-motor symptoms like hallucinations, confusion, or excessive daytime sleepiness. The other four look at motor symptoms such as stiffness, slow movements, and balance issues. It helps doctors identify possible signs of LBD early, but it’s not a diagnosis on its own.